Background and Objectives: Relapsed/refractory (R/R) primary and secondary central nervous system lymphomas (PCNSL, SCNSL) are associated with short survival and represent an unmet need, requiring novel effective strategies.
Methods: We retrospectively compared the safety and efficacy of CD19/22 CAR T-cell therapy combined with HDT-ASCT (ASCT+CAR-T group), CD19/22 CAR T-cell cocktail therapy (CAR-T group) and targeted drugs combined with chemotherapy (Targeted drugs group) in treating R/R CNSL patients.
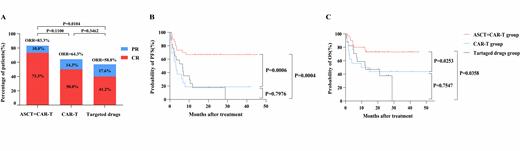
Results: The median age of the Targeted drugs group is older than that of the other two groups, 73.3%, 100% and 41.2% patients were secondary CNS lymphoma in ASCT+CAR-T group, CAR-T group and Targeted drugs group, respectively. The incidence of Grade 3/4 hematological toxicities in ASCT+CAR-T and CAR-T group was more than Targeted drugs group. Patients in two CAR-T therapy group exhibited comparable incidence and severity of CRS and ICANS. The ORR was 83.3% in ASCT+CAR-T group, 64.3% in CAR-T group and 58.8% in Targeted drugs group respectively (Figure 1). As of December 31, 2022, the median follow-up time after therapy was 15.53 months (range, 0.53-50.53 months). The median duration of OS and PFS was not reached in the ASCT+CAR-T group. The median PFS and OS in the CAR-T group were 3.07 months and 9.67 months, respectively. In the Targeted drugs group, the median PFS and OS were 6.63 months and 12.30 months, respectively. The 1-year PFS and OS rate of the patients in the ASCT+CAR-T group (66.67% and 76.52%) was significantly higher than that of the patients in the CAR-T group (18.75% and 50%) ( P=0.0006 and P=0.0253) and targeted drugs group (17.65% and 52.94%) ( P=0.0004 and P=0.0358) (Figure 1). In both univariable and multivariate analysis, PD before treatment was indicated worser PFS (HR: 3.134, 95% CI, 1.144 to 8.587, P=0.026), rather than OS, both in ASCT+CAR-T and CAR-T group and compared with CAR-T group, patients received ASCT+CAR-T treatment had better PFS (HR: 0.279, 95% CI, 0.120 to 0.651, P=0.003), rather than OS. PFS and OS of patients with PD before treatment, patients with ECOG ≥2, with high risk factors, and with>3 prior lines of therapy in the ASCT+CAR-T group were superior to CAR-T group (Supplementary Figure 1). In the ASCT+CAR-T group, PFS, rather than OS, of patients without systemic disease in the ASCT+CAR-T group was superior to those with systemic disease ( P=0.0335).
Discussion: Our results support the development of CAR T -cells in R/R CNSL. With the durability of remission and low toxicity, ASCT combined with CART therapy appears to be a more effective and safe treatment option for primary and secondary relapsed/refractory CNS lymphoma.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal